Vascular care has come a long way
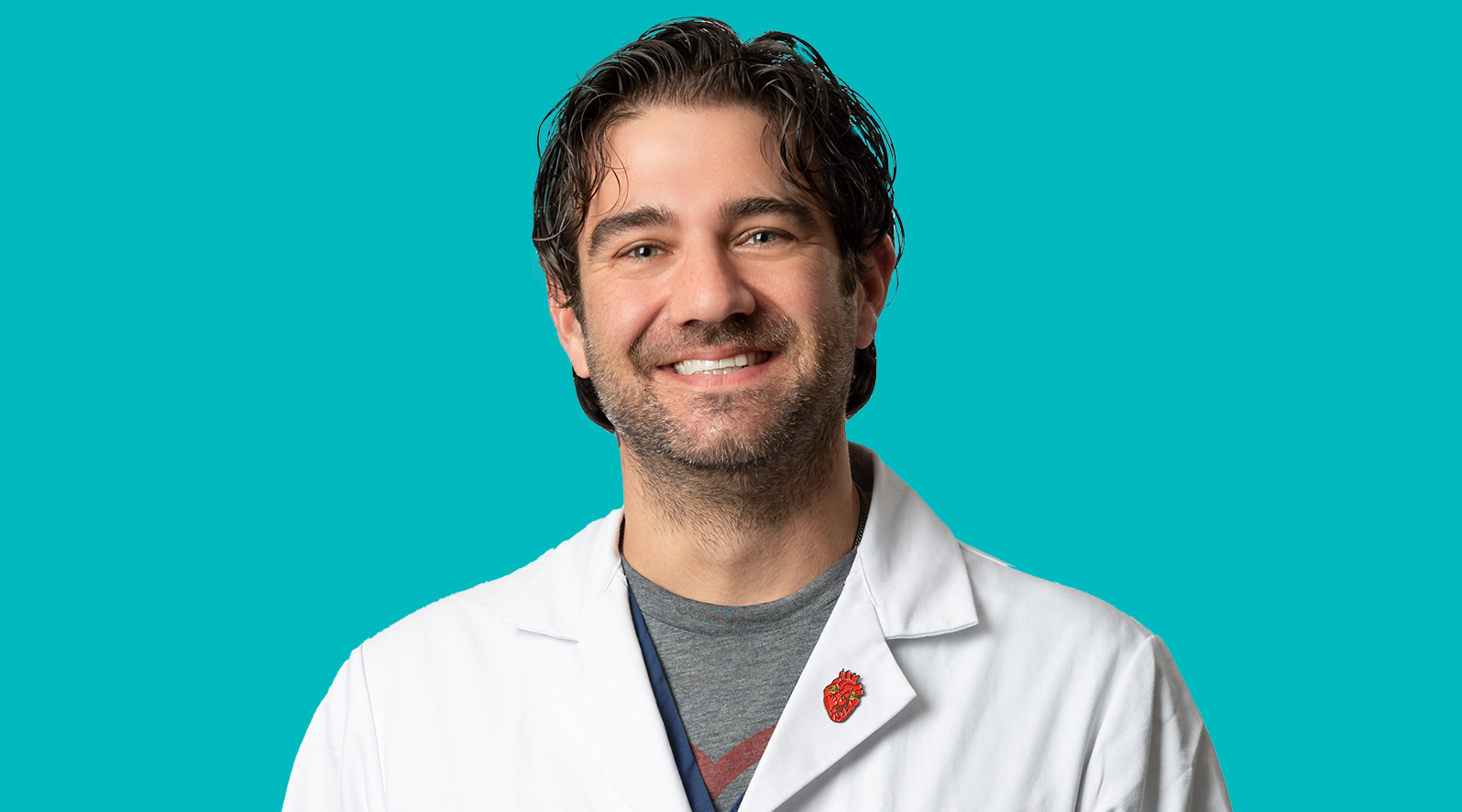
“Approximately 60 to 70 percent of vascular surgery procedures are performed with a minimally invasive approach,” says Michael Singh, MD, chief of Surgical Services and chief of Vascular Surgery at UPMC Shadyside, and co-director of the UPMC Heart and Vascular Institute Aortic Center.
Dr. Singh explains that “vascular surgeons have the ability to manage conditions that affect the arteries, veins, and lymphatic system from the head down to the toes. The exception is the heart, which is best managed by the cardiology and cardiothoracic surgery teams.”
Dr. Singh’s area of expertise is the thoracic and abdominal aorta, the main blood vessel emanating from the heart and extending into the abdomen, where it bifurcates to the left and right iliac arteries. For a variety of reasons, the aorta can develop stenoses, dissect, or degenerate, which is called an aneurysm. It represents a focal weakening of the blood vessel wall and leads to a dilation of the vessel. This can be a very serious condition, because if an aneurysm ruptures, the mortality rate is between 80 and 90 percent.
Traditionally, aneurysms have been managed with large incisions to perform open surgical repair. “However, the standard of care has changed,” Dr. Singh says. “Patients often request ‘the least invasive way to fix my aneurysm that is not going to change my long-term quality of life.’ The good news is that we can offer patients a less invasive aneurysm repair where they can essentially walk out of the hospital the following morning with nothing more than a small bandage covering the needle puncture on the top of both thighs. It’s a tremendous advancement in patient care. These less invasive treatment options improve patient care, reduce recovery time, shorten hospital length of stay, and reduce the risk of future aneurysm rupture. These less invasive repairs can be offered for aneurysms in the chest, abdomen, and pelvis.”
Dr. Singh oversees several aortic clinical trials that are underway and acknowledges that such trials will “expand treatment indications and hopefully improve vascular care for all patients.
“People deserve to receive high-quality care performed at a spectacular institution, which Shadyside is,” Dr. Singh states. “We’re very fortunate to have state-of-the-art resources and cutting-edge technology here. UPMC is at the leading edge of technology advancement, and we expect to stay there for many decades to come.”